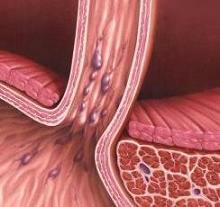
 Varicose veins of the esophagus - a term denoting a venous expansion in the lower part of the esophagus, which is the result of blood flow disorders in the portal vein and, consequently, the gastroesophageal plexus by an excessive amount of flowing blood, which seeks an outflow from the heart.
Varicose veins of the esophagus - a term denoting a venous expansion in the lower part of the esophagus, which is the result of blood flow disorders in the portal vein and, consequently, the gastroesophageal plexus by an excessive amount of flowing blood, which seeks an outflow from the heart.
In connection with the fact that with varicose veins of the esophagus in 90% of cases corresponds to cirrhosis of the liver, yellowing of the skin and eye proteins, loss of appetite, weight loss, ascites, abdominal pain and nausea.
The most dangerous symptom of this disease is associated with hemoptysis, mixed with blood vomiting, tarry stool and weakness.
Causes
Varicose esophagus in its lower part arises because of stagnant phenomena in the portal portal vein system that occur with thrombosis and cirrhosis of the liver. The cause of this disease in the upper division is malignant goiter. The veins of the liver contract, which makes the blood flow difficult for them. Phlebectasia of the esophagus also appears as a complication in diseases of the heart and spleen.
Factors, causing this disease:
- stenosis of the portal vein, characteristic of the younger generation, resulting from thrombosis, sclerosis;
- liver diseases that occur in advanced age - cirrhosis, amyloidosis, echinococcosis;
- Chiari's disease;
- esophagus angioma;
- malignant goiter;
- cardiovascular pathology.
Varicose veins of the esophagusmost often occurs in the following categories of patients:
- in men;
- in people over 50;
- in patients with a history of pancreas, stomach, heart, chronic cirrhosis.
The appearance of bleeding is affected not so much by the level of pressure as by its sharp fluctuations. The risk of rupture is high also in those patients who suffer from vascular diseases, negatively affecting the structure of the walls of blood vessels.
Classification
Classification of the disease of varicose veins of the esophagus has changed several times, however, the version from 1997 for the esophagus veins that divides the disease according to the degrees is now used:
- First degree. The veins in diameter reach 5 mm, markedly elongated, located in the lower level of the organ.
- Second degree. The veins are convoluted, in diameter reach 10 mm, located in the middle part of the organ.
- Third degree. Vessels are expanded more than up to 10 mm, the walls are tense, thin, located side by side, winding in the direction, have red spots on the outer surface.
If varicose veins of the esophagus still caused internal bleeding, then according to statistics - after it only 50% of patients survive. More than half of the survivors after bleeding suffer from the disease for 1-3 years with relapse of this disease and are forced to start treatment again.
Varicose veins of 1 degree
The clinical picture is poorly expressed. The patient has practically no complaints. At inspection observe: the expansion of veins not strong up to 3 mm., Ectasia of veins is not present, or only single, the gleam is not filled. It is only diagnosed with endoscopy. At the first degree it is important to begin treatment as soon as possible.
Varicose veins of the 2nd degree
Well observed irregularity of the vessels, as well as there are nodules, the size of which exceeds 3 millimeters. In this case, the mucosa of the esophagus remains intact, without any violation of its integrity.
During the study, it is possible to diagnose large vessels in protrusions. Treatment should be done in a timely manner, only in this way it will be possible to get rid of the unpleasant symptoms of the disease at the initial stage. Bleeding is not typical at this stage.
Varicose veins of the 3rd degree
The most common diagnosis. The patient has severe symptoms. As a rule, in this case, an operation is appointed. The veins are strongly swollen, the nodes clearly appear, constantly enlarged, occupy 2/3 of the esophagus, the mucosa of the esophagus is severely thinned. There are gastroesophageal refluxes.
Varicose veins of the 4th degree
This degree of disease is exhibited when numerous nodules of veins are revealed in the esophagus that do not subside and have a thin surface. Numerous erosions are found on the mucous layer. Patients register, in addition to the symptoms of esophagitis, a salty taste in the mouth. The fourth degree most often leads to spontaneous bleeding.
Symptoms of varicose veins of the esophagus
The first few years, the varicose veins of the esophagus can flow without any visible symptoms. Sometimes there are rare attacks of heartburn, a weak heaviness in the chest, belching. Some patients complain of difficulty with swallowing food.
Symptoms of progressive disease usually appear several days before the onset of bleeding. Signs of them consist in severe heaviness in the chest and deterioration of the general well-being of the patient. In other patients, symptoms can be expressed in the manifestation of ascites.
In addition, symptoms of venipuncture of the esophagus may appear as the appearance of a "jellyfish head". This phenomenon is a certain pattern, which is rather well seen on the anterior wall of the abdominal cavity by various pathologically formed convex vessels or veins.
After the veins burst, there is a severe bleeding, accompanied by characteristic symptoms:
- greatly reduced blood pressure;
- bloody impurities in vomiting;
- bloody impurities in feces;
- marked tachycardia.
With a slight bleeding, a person may feel some weakness, malaise, as well as symptoms of anemia. Diagnosis of esophagus varicose with the help of laboratory tests, ultrasound examination of the abdominal cavity organs, if necessary, conduct X-ray studies and esophagoscopy.
Diagnostics
The diagnosis is made on the basis of complaints, external examination, detection of primary diseases. Instrumental studies include:
- laboratory blood test data;
- radiography with contrast medium;
- Esophagoscopy which must be done carefully because of the risk of possible bleeding.
When making a diagnosis, all possible causes should be taken into account and excluded, only then it will be possible to definitively and accurately determine the root cause of bleeding and changes in the esophagus.
Treatment of varicose veins of the esophagus
If there are symptoms of varicose veins of the esophagus, treatment is performed only in the intensive care unit. The main classification of non-surgical procedures is aimed at preventing and eliminating bleeding (haemostatic therapy) by reducing pressure in the vessels:
- Medicamentous treatment in the form of vitamins, astringents and antacids (drugs that reduce acidity in the stomach). This method is aimed at the prevention of peptic esophagitis, in which inflammation can go to the walls of the vessels, causing bleeding.
- Transfusion of blood, erythrocyte mass, plasma;
- Introduction of colloidal solutions;
- Reception of blood-reducing and vasoconstrictive drugs.
In cases where these methods are not sufficient for a thorough stopping of bleeding and there is a risk of repeated damage to the vessels in the near future,resort to surgery:
- transgular intrahepatic portosystemic shunting (TIPS);
- shunting;
- devascularization.
Also, there is now considerable experience in the use of minimally invasive endoscopic interventions to eliminate bleeding from the enlarged esophageal veins. There are 2 ways of carrying out endoscopic sclerotherapy of the esophagus:
- intravasal;
- paravalous.
The intravasal method of introducing sclerosant involves the development of connective tissue at the site of localization of the thrombosed varicose node. In the paravasal method, when the sclerosant is injected into the submucosal layer, scarring of paravasal tissue and subsequent compression of the enlarged esophagus veins occurs. This method is more sparing and has fewer complications.
Diet
Patients need to follow a strict diet all their life, despite the state of health:
- frequent meals in small portions.
- Exclusion of hot and cold dishes.
- shows low-fat broths and soups, cereals in diluted milk or water, compotes, fruit in a grinded form, vegetables stewed.
- contraindicated acute, acidic, salty, fatty and fried meat products; it is necessary to cook everything in a puree.
Categorically contraindicated alcohol, carbonated drinks, beer.
Prevention
To prevent the transformation of healthy esophagus veins into pathological, varicose veins, first of all it is necessary to monitor the liver and timely treat all of its diseases. To do this, experts advise to consult them regularly for advice and follow all recommendations.
Forecast for life
Unfortunately, varicose veins of the esophagus are incurable. However, in the case of timely diagnosis, adequate maintenance treatment will significantly improve the quality of life of the patient and help prevent a formidable condition - bleeding.
Mortality in the already existing bleeding from varicose veins of the esophagus is more than 50% and depends on the severity of the underlying disease and the state of the organism as a whole. In surviving patients after bleeding in 75% of cases within the next 1-2 years there is a relapse.
In general, the prognosis of long-term survival of patients with this disease remains low, which is mainly the fault of the main severe liver disease.

How to choose probiotics for the intestine: a list of drugs.

Effective and inexpensive cough syrups for children and adults.

Modern non-steroidal anti-inflammatory drugs.

Review of tablets from the increased pressure of the new generation.
 Antiviral drugs are inexpensive and effective.
Antiviral drugs are inexpensive and effective.



