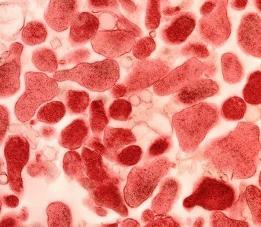
 Mycoplasma in women is a microorganism occupying an intermediate position between bacteria, fungi and viruses.Usually, mycoplasma is attached to epithelial cells - the lining of the lining of the intestinal, respiratory and genito-urinary tracts. Parasitize in host cells.
Mycoplasma in women is a microorganism occupying an intermediate position between bacteria, fungi and viruses.Usually, mycoplasma is attached to epithelial cells - the lining of the lining of the intestinal, respiratory and genito-urinary tracts. Parasitize in host cells.
On reception at the gynecologist even absolutely healthy woman can receive on hands results of analyzes where mycoplasma is found out. Conditionally pathogenic flora, which doctors take into account only under the condition of high titers, is quite common.
If the growth of the flora is very active and there are prerequisites for reducing the immune system, then a diagnosis is made - mycoplasmosis. Let's deal with you what it is, and what methods of treatment can overcome these microorganisms.
Causes
Why does mycoplasma develop in women, and what is it? Mycoplasma is considered the smallest form of organisms belonging to the family mycoplasmataceae. It is referred to as an intermediate between unicellular organisms and multicellular viruses and bacteria.
Despite this, scientists tend to regard them (mycoplasmas) as viruses, since they do not have a cell membrane. In the family mycoplasmataceae, there are two kinds of microorganisms, mycoplasma and ureaplasma, which can cause a variety of diseases.
The source of infection is a person with a manifest or asymptomatic course of mycoplasmosis. Infection is transmitted by airborne (with respiratory mycoplasmosis), sexual (with urogenital mycoplasmosis) and vertical (from mother to fetus - more often with urogenital mycoplasmosis) ways.
The incubation period of the disease is from 3 days to 5 weeks, an average of 15-19 days.
Symptoms of mycoplasma in women
 As a rule, the presence of mycoplasmas in the body is characterized by erased malosymptomatic forms. Approximately 10-20% of women do not feel any obvious symptoms of mycoplasma, until a stressful situation, for example, abortion or severe hypothermia, do not activate the infection, often leading to serious complications.
As a rule, the presence of mycoplasmas in the body is characterized by erased malosymptomatic forms. Approximately 10-20% of women do not feel any obvious symptoms of mycoplasma, until a stressful situation, for example, abortion or severe hypothermia, do not activate the infection, often leading to serious complications.
Often the acute form of the disease is preceded by the incubation period, and only 7-10 days after infection the first signs of mycoplasmosis may appear:
- With defeatexternal genitaliaparasites accumulate on the mucous membrane of the vagina and the urethra. In such a situation, patients usually do not make any complaints. Sometimes it is possible the emergence of a mild itching of the external genitalia and the appearance of lean colorless secretions from the genital tract.
- Whenpenetration of infection into the internal genital organsthere are pains in the lower abdomen, burning and itching during urination, abundant, sometimes purulent, discharge from the genital tract.
Urogenital mycoplasmosisin women is manifested in the form:
- bacterial vaginosis (gardnerellosis);
- Mycoplasma urethritis;
- inflammation of the uterus, fallopian tubes and ovaries;
- pyelonephritis;
- often mycoplasmosis is combined with chlamydia and ureaplasmosis.
The insidiousness of mycoplasma in women lies in the fact that the disease for many years can be completely asymptomatic. During this period, the woman is the carrier of the infection and can pass it on to her sexual partners.
Diagnostics
Diagnosis of urogenital mycoplasmosis is based on the PCR method (polymerase chain reaction), in which the DNA of mycoplasmas is determined. Also, a classical culture method is used, with the sowing of the material on a liquid medium and the subsequent re-entry into a solid one.
Mycoplasma is determined from the fluorescence of the colonies after the addition of specific anti-sera. Serological methods for detection of mycoplasmas - complement fixation reaction (RSK) and indirect agglutination reaction (RNGA).
As a material for laboratory research, women take a swab from the cervix, vestibule, urethra and anus, the morning portion of the first urine.
Treatment of mycoplasma in women
When diagnosing mycoplasma in women, the treating physician prescribes a treatment regimen consisting of complex therapy, which includes:
- Antibacterial drugs(in connection with the resistance of mycoplasma to penicillin, antibiotics for mycoplasmosis are used from the group of tetracycline, and also macrolides are used, the course of this treatment is up to 2 weeks);
- Local treatment (suppositories, syringing);
- Immunomodulators (these drugs enhance the effect of drugs, use in the treatment of tsikloferon or lycopide);
- Compliance with a doctor's recommended diet;
- Physiotherapy.
Unfortunately, the human body is not able to develop immunity to this infection, and therefore, both sex partners need to be treated with the drugs simultaneously. On average, the course of treatment of mycoplasmosis is 10 days. Then, after 2 or 3 weeks, the patient is assigned bacussis, and after 30 days - PCR.
Chronic form
In the treatment of chronic forms, immuno-focused and topical therapy is of great importance. The goal of immuno-targeted therapy is to correct the immunodeficiency state, which became the cause of the chronic course of the disease and intensified against its background. It is appointed taking into account the immunogram indices.
Local therapy is carried out simultaneously with systemic antibiotic therapy, for 5-7 days. Usually, ethmotropic, anti-inflammatory agents and enzymes (trypsin, chymotrypsin, etc.) are usually prescribed in the form of installations or using cotton-tampons for the treatment of the vagina. Immediately after its completion, it is recommended to undergo a course of treatment with probiotics to restore microflora.
Effects
A prolonged course of mycoplasmosis without symptoms leads to the development of endometritis - inflammation of the uterine mucosa. In women with mycoplasmal endometritis, miscarriages and stiff pregnancies are frequent.
From the uterus M. hominis and M. genitalium can spread to its appendages with the development of adnexitis. Then spikes appear in the tubes, which can lead to an ectopic pregnancy.

How to choose probiotics for the intestine: a list of drugs.

Effective and inexpensive cough syrups for children and adults.

Modern non-steroidal anti-inflammatory drugs.

Review of tablets from the increased pressure of the new generation.
 Antiviral drugs are inexpensive and effective.
Antiviral drugs are inexpensive and effective.



