- What you need to know about gastroduodenitis?
- Menu requirements for gastroduodenitis
- What is the classic diet by the number that corresponds to gastroduodenitis?
- What products are excluded from food?
- What can I eat?
- Features of table options №1
- How to organize proper nutrition for a sick child?
- How to eat a patient without exacerbation?
- What is atrophic form without increased acidity?
- Related videos
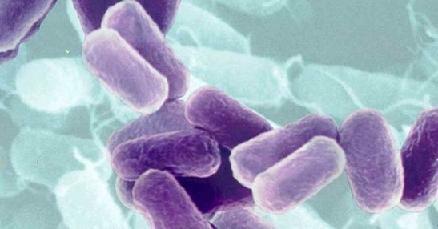
Simultaneous inflammation of the stomach and bulb of the duodenum( gastroduodenitis), according to medical statistics, is found in half of the adult population.
It is important that the disease quickly captures the environment of children and adolescents, in 70% of cases it immediately acquires a chronic course. The importance of diets with gastroduodenitis is paid attention to by all gastroenterologists. Without proper phased dietary nutrition, it is impossible to achieve positive results in treatment.
What you need to know about gastroduodenitis?
Gastroduodenitis is caused by many causes. Leading role belongs to violations in human nutrition. What matters is:
- a propensity for the predominant use of coarse fried and fatty meat foods;
- failure of the regime( especially painfully tolerated by children);
- suffered food poisoning;
- alcohol;
- intolerance of any food.
People with gastroduodenitis often suffer from unbalanced people, after suffering stress, increased stress at work or in school. The disease is a consequence of the use of chips, carbonated water, snacks in the dry. More and more cases are associated with the negative effects of drugs.
Inflammation in gastroduodenitis is localized in the border zone( pyloroduodenal).It is here that hormonal substances are produced that are responsible for reducing the acid reaction during the passage of the food lump through the sphincter into the small intestine.
Dysregulation leads to a stable state of increased acidity, throwing gastric juice into the bulb zone. There is an erosion of the acid mucosa of the duodenum in the upper parts. Very rarely, the disease is detected with reduced or normal acidity.
If the process captures the entire gut, then dangerous conditions are created for involving the pancreas( pancreatitis) and bile ducts( cholangitis) in the inflammation, since they are connected by a common duct. With chronic gastroduodenitis, these pathological changes are inevitable. Therefore, a diet with duodenitis and gastritis is necessarily formed taking into account the effect on the entire digestive tract.
Acute form of inflammation is most typical for poisoning, the child can be accompanied by an infectious disease. Symptoms reflect a primary lesion of the stomach( pain immediately after eating or a little later, heartburn, belching) or duodenal ulcers( nocturnal or "hungry pains").
The easy course( superficial gastroduodenitis) allows you to limit therapy to adherence to strict dietary rules in choosing a menu for up to a month. If the diagnosis reveals an erosive form, then nutrition with gastroduodenitis as close as possible to the composition of peptic ulcer.

The benefits of vegetables are not fully preserved when boiled
Menu requirements for gastroduodenitis
The composition of the products in the menu and the methods of processing food should lead to the creation of the most sparing dishes. It is necessary to prevent irritation of the mucous membrane of the stomach and intestines with heavy products in terms of chemical composition, as well as causing increased littering.
For this purpose gastroduodenitis is prohibited from cooking by roasting, smoking, only dishes cooked with boiled, stewed, steamed are allowed.
Do not allow large amounts of food to enter the stomach, overeating, long breaks in food. A balanced menu should take into account that you can eat no more than 150 grams of food at a time. It is required to follow the schedule of frequency of a food on 5-6 times a day.
Too cold or hot food is also an unnecessary stimulus for acid production. Cooked meals can be eaten warm. The most optimal temperature is 38-40 degrees. It ensures the safe absorption of useful nutrients and does not cause additional traumatization of the mucosa in patients with gastroduodenitis.
For mechanical shchazheniya all meals to the patient at the stage of exacerbation appoint rubbed or twice scrolled through a meat grinder. Up to 40% of cases of gastroduodenitis occur atypically, there are no intense pains, patients do not note heartburn. For them, there is no need for strict observance of the mechanical treatment of products, but all contraindications on the composition of the food are effective.
What is the classic diet according to the number corresponding to gastroduodenitis?
A special table in Pevsner's classification for gastroduodenitis is not provided. Recommending an approximate diet, the doctor is guided by the predominant symptomatology, data of fibrogastroscopy, signs of simultaneous damage to the pancreas. Usually acute stage treatment begins with table 1 options. Successively apply 1a and 1b.
This diet is also prescribed for peptic ulcer, postoperative period with surgical intervention on the stomach and intestines, acute and chronic gastritis. To achieve positive dynamics in treatment, this diet is most suitable for gastroduodenitis( it provides healing, mucosal shining, normalization of acidity).

The correct food schedule should coincide with the intensity of the metabolism of
. In addition to the general requirements, Table No. 1 recommends:
- introduce a restriction on table salt( up to 10 g / day) and salty foods;
- provide for a sufficient caloric content of the daily diet;
- include in the composition the required amount of carbohydrates, proteins, fats, vitamins and trace elements.
When spreading the inflammatory process to the bile ducts, a malfunction of the pancreas can be combined with diet number 5. Table 5a differs little from the first, but table 5n will require reduced fat and sugar replacement for xylitol, more precise control of protein content.
What products are excluded from food?
Table number 1 is quite strict, all the prohibitions must be fulfilled. The patient is contraindicated:
- rich fish and meat broths, soups;
- any dishes from cabbage and mushrooms;
- fat, sausages;
- canned food;
- fatty meat and fish products, fried dishes from them;
- raw vegetables;Acid fruits and berries, juices;
- gooseberry, grapes;
- spicy seasonings, sauces, mayonnaise, spices, ketchup;
- onion, any greens, garlic,
- sweet bread, fresh pastries, rye flour products;
- sparkling water;
- coffee;
- alcoholic beverages;
- chocolate;
- ice cream.
What can I eat?
The need for caloric content and nutrients should be provided by milk. This product has all the necessary properties( the necessary content of protein, fat, vitamins, alkalinization), some people have intolerance, bloating. Milk porridge is prepared on diluted milk.

The signs of intolerance can be eliminated if you add milk to tea, dilute it, drink it only in small sips in a warm form.
Calculation of a diet includes at least 30% of refined vegetable oils( olive or sunflower) in the fat composition. Fish and meat dishes are only allowed to be grated, cooked or baked, steamed meatballs, meatballs, soufflé.Vegetables are used in broth, vegetarian soups, necessarily wiped. Thin pasta should be boiled. Bread can only be dried wheat.
Features of table options №1
Table No. 1a - recommended for exacerbation of gastroduodenitis during the first week of therapy. Usually the patient is in hospital and the composition of the products is monitored by the dieter. The option provides the maximum conditions for shining for the stomach and intestines. In just a day you can eat 2.5 kg of food, calorie limit 2200 kcal. In the diet, proteins are reduced to 80 grams, carbohydrates - to 200 g.
To the patient prepare liquid porridges on water or diluted milk from oatmeal, rice( buckwheat and millet are not recommended), milk soup with small vermicelli, meat soufflé, jelly from non-acid berries. One egg is allowed to soften, or in a scrambled omelette, freshly ground cottage cheese. For drinking - a decoction of rose hips.
On the table number 1b - you can go on average after a week or ten days. The menu increases the amount of protein to 100 grams, carbohydrates to almost normal( 400 g), the total weight of food per day is reduced to 2.5-3 kg, and caloric content - up to 3000 kcal. Food remains semi-liquid, but vegetable mashed potatoes, stewed vegetables with meat, meatballs and steamed meatballs, buckwheat, rice and oatmeal with a little sugar or honey added are allowed.
Full table number 1 - follows option 1b. If all restrictions are met, daily diets of food are increased to 3-3.5 kg. There remain requirements for the methods of preparation. Permitted milk noodles and vermicelli, omelet from eggs, low-fat kefir( two glasses a day) is added. Kalorage allows 3200 kcal, and the composition is almost brought to normal.

5 g of butter is added directly to the plate
How to organize proper nutrition for a sick child?
The peculiarity of gastroduodenitis in children is the undulating course of the disease. The basic requirements for products and methods of processing, the feeding regime do not differ from adult nutrition. Parents need to organize diet control for one and a half to two years. This time is necessary for teaching the child the skills of proper nutrition, explaining the harm from eating dry foods, chips, fast food, carbonated drinks.
The diet for gastroduodenitis in children is more often associated with acute inflammation amid food poisoning, infectious gastroenteritis. The period of strict limitations depends on the severity of the disease and the lesions of the gastrointestinal tract.
The approximate menu for the day should include all age standards for caloric content with a temporary restriction of fats, carbohydrates, because in almost every case, children are not excluded from the possibility of failure of the pancreas. The child's diet is formed by the day. We give an example of nutrition for a week.
Day One
It is recommended to observe a hunger regime, but often to give the child a warm broth of rose hips, weakly boiled tea.
The second day
To the plentiful drink is added rice or vegetable broth, white crackers, oat jelly.
Day Three
Liquid rice or oatmeal in diluted milk is allowed, it is better to grind the groats first. In a ready dish you can put no more than 5 g of butter. To the tea is added a dry biscuit.
Day four
For breakfast and dinner there are porridges. For lunch, vegetable soup is prepared in the form of liquid puree from potatoes, carrots, pumpkins, which is refilled with creamy or unrefined vegetable oil. You can add white crackers. To an afternoon snack a baked apple is allowed.
Day Five
Dietary diet is expanding due to:
- variety of vegetable purees with butter;
- of meatballs or meatballs;
- fermented milk products( kefir, yogurt, low-fat, wiped cottage cheese).
Unsweetened biscuits, dry biscuits are allowed for tea.
Day of the sixth
We give an example of a menu.
For the first breakfast - you can give milk porridge porridge or curd casserole with fruit, a little sweet tea.
For the second breakfast - fruit or vegetable puree.
For lunch - the first dish is prepared from fresh vegetables, low-fat fish;the second - steam chicken cutlets( nutritionists recommend mixing ground grated carrots or pumpkin);white bread dried, compote of dried fruits.
For a snack, milk or kefir with a dry biscuit or stewed apple without skin is suitable.
For dinner - vegetable puree can be alternated with cottage cheese, it is allowed to fill it with low-fat sour cream and add a little sugar. To drink food is recommended decoction of rose hips or compote.
At night, children like to drink kefir or yogurt.

Abandonment of bad habits, alcohol, organization of high-quality nutrition - an indispensable condition for preventing exacerbations
How to eat without exacerbation?
After the elimination of acute symptoms, the further course of gastroduodenitis largely depends on the patient's exposure. The patient will have to get used to:
- dispense with food that irritates the mucous;
- drink more fluids;
- to the exclusion of pickles, marinades, canned hot sauces and spices;
- to the lack of onions and garlic, pearl and millet porridge, fresh fruits and vegetables, strong coffee and tea.
What is atrophic form without increased acidity?
This type of disease is considered rare. It is widely believed that atrophy occurs when cells that produce hydrochloric acid are depleted. Therefore, we have the right to assume that in the course of a prolonged course, the hyperacid pathology passes to normal and then decreased acidity.
In the diet there are all requirements aimed at protecting the surface of the stomach and duodenum( mechanical processing, boiling, banning frying).Some nutritionists allow frying without breadcrumbs, grinding only rough products.
At the atrophic form of gastroduodenitis diet table №2 is shown. It is able not only to heal damage to the mucosa, but also to promote the recovery of the secreting function of cells. Therefore, in the menu must be present:
- meat and fish broth;
- borsch, beetroot, shchi, pickle without pickled cucumbers;
- boiled vegetables in fresh form for first courses and boiled for the second;
- more salty products than with increased acidity;
- compote and jelly from moderately acidic berries, fruits;
- cheese cakes and vareniki with cottage cheese or potatoes;
- liver pate;
- tomatoes, greens;
- cooked sausage;
- jellied fish;
- salads from boiled vegetables;
- lightly salted herring;
- sufficient volume of liquid in the prohibition to wash down food with water.
It is allowed to drink tea with lemon, not strong coffee, oranges or tangerines, grapes without skin, watermelon. The issues of nutrition, the problem of organizing frequent snacks are especially difficult for working people, students. But without a proper diet, treatment does not make sense, the disease leads to complications.